Urine Analysis: Key Characteristics and Insights
Pathology Unit 5: Urine and Feces
Short Essay
Examination Done on Urine
- Urine testing is also known as urinalysis.
Physical Characteristics
1. Color
- Dark colored urine: May indicate excessive sweating, dehydration, or reduced fluid intake.
- Insight: Dark urine can be a sign of insufficient hydration.
- Light colored urine: Suggests excessive fluid intake or certain renal conditions.
- Insight: A lighter color usually implies good hydration levels.
- Bright yellow urine: Often due to Vitamin B supplements.
- Insight: Bright yellow may be normal with supplements but might also indicate excessive intake.
- Red-brown urine: Could be due to certain medications, blackberries, or the presence of blood.
- Insight: Persistent red-brown urine should be medically evaluated.
2. Clarity
- Normal urine clarity: Generally clear.
- Insight: Cloudiness often indicates an issue.
- Cloudy urine causes: Bacteria, blood, sperm, etc.
- Insight: Cloudiness can suggest an infection or other pathology.
3. Odor
- Fruity odor: May be caused by Diabetes Mellitus (DM).
- Insight: Fruity-smelling urine often relates to ketone bodies in diabetes.
4. pH
- High (alkaline) pH: Could be due to severe vomiting or a urinary tract infection (UTI).
- Insight: Alkaline urine might signify a body's response to imbalance or infection.
- Low (acidic) pH: May indicate diabetes, diarrhea, or excessive alcohol consumption.
- Insight: Acidic urine can be a response to metabolic or dietary factors.
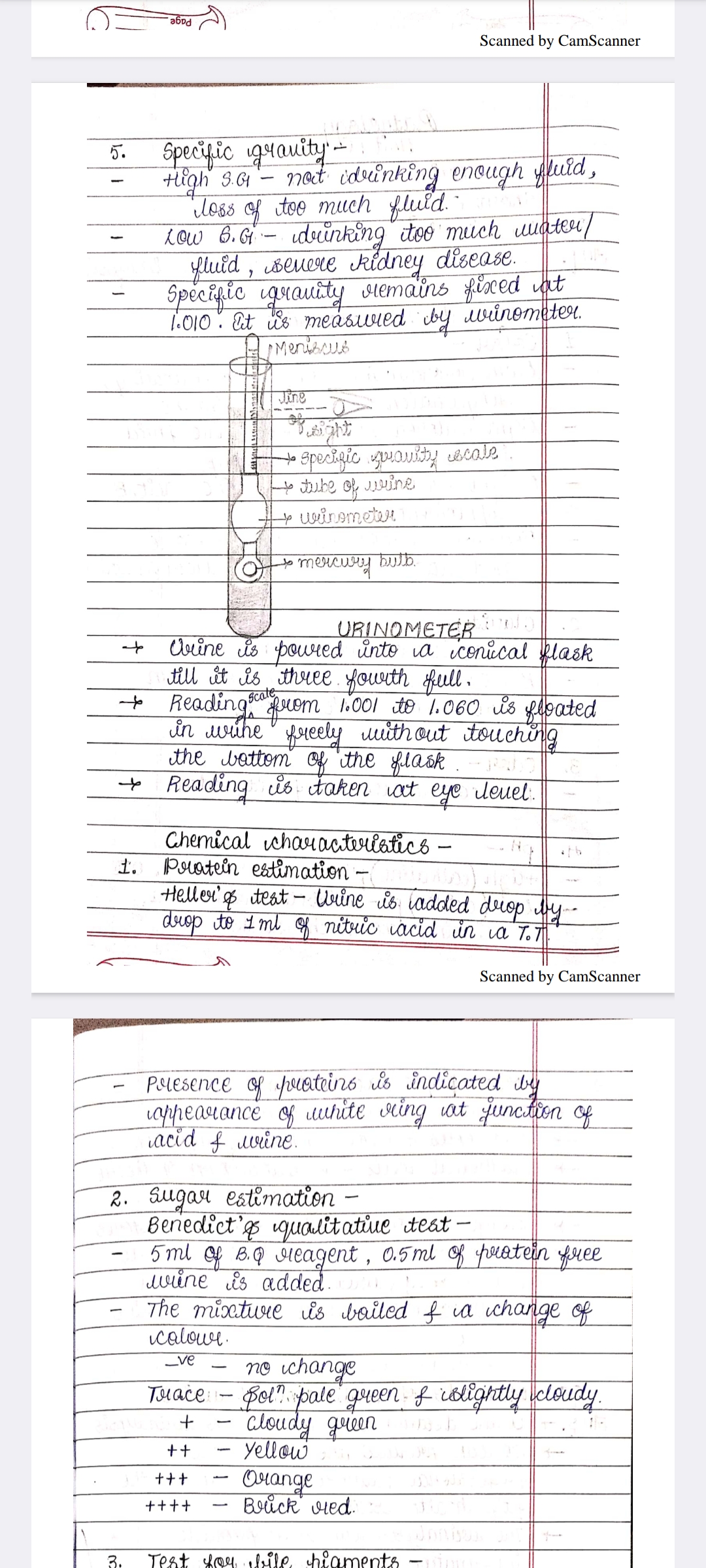
5. Specific Gravity
- High S.G.: Suggests not drinking enough fluid, possibly due to fluid loss.
- Insight: High specific gravity indicates concentrated urine.
- Low S.G.: Can be a result of drinking too much water or severe kidney disease.
- Insight: Low specific gravity signifies dilute urine, commonly seen in overhydration or kidney issues.
- Fixed Specific Gravity at 1.010: Indicates kidney disease.
- Insight: Fixed specific gravity can indicate renal dysfunction, unable to concentrate or dilute urine.
- Measurement tool: Urinometer.
Diagram Explanation
The diagram includes a measurement of specific gravity using a urinometer. It helps in identifying the density of urine compared to water and determining fluid balance and kidney function.
Extended readings:
Urinalysis Notes
Specific Gravity
-
High Specific Gravity:
- Causes: Not drinking enough fluids, loss of fluids.
- Insight: Indicates concentrated urine; possible dehydration.
-
Low Specific Gravity:
- Causes: Drinking excess fluids, severe kidney disease.
- Insight: Suggests dilute urine; monitor fluid intake and kidney function.
-
Fixed Specific Gravity (1.010):
- Insight: May point to severe renal impairment where kidneys cannot concentrate urine effectively.
-
Measurement Method:
- Urinometer: Device used for measuring the specific gravity of urine.
- Diagram Components:
- Meniscus, scale, urinometer tube, mercury bulb.
- Insight: Evaluates kidney function and fluid balance in the body.
Urinometer Procedure
- Steps:
- Fill a conical flask with urine until it is three-fourths full.
- The urinometer floats freely without touching the flask's bottom.
- Read the scale at eye level.
Chemical Characteristics
1. Protein Estimation
- Heller's Test:
- Method: Add urine drop by drop to 1ml of nitric acid.
- Presence Indicator: A white ring at the junction if proteins are present.
2. Sugar Estimation
- Benedict’s Qualitative Test:
- Method: Mix 5ml of Benedict's reagent with 0.5ml of protein-free urine and boil.
- Color Change Indicators:
- (-): No change
- Trace: Very pale green, slightly cloudy
- (+): Cloudy green
- (++): Yellow
- (+++) Orange
- (++++): Brick red
- Insight: Color change indicates the presence and concentration of reducing sugars.
3. Test for Bile Pigments
- Insight: Helps in diagnosing liver dysfunction by detecting the presence of bile pigments in urine.
These notes provide a structured insight into urinalysis, covering specific gravity and key chemical characteristics used to evaluate overall health status.
Extended readings:
Antiemetics
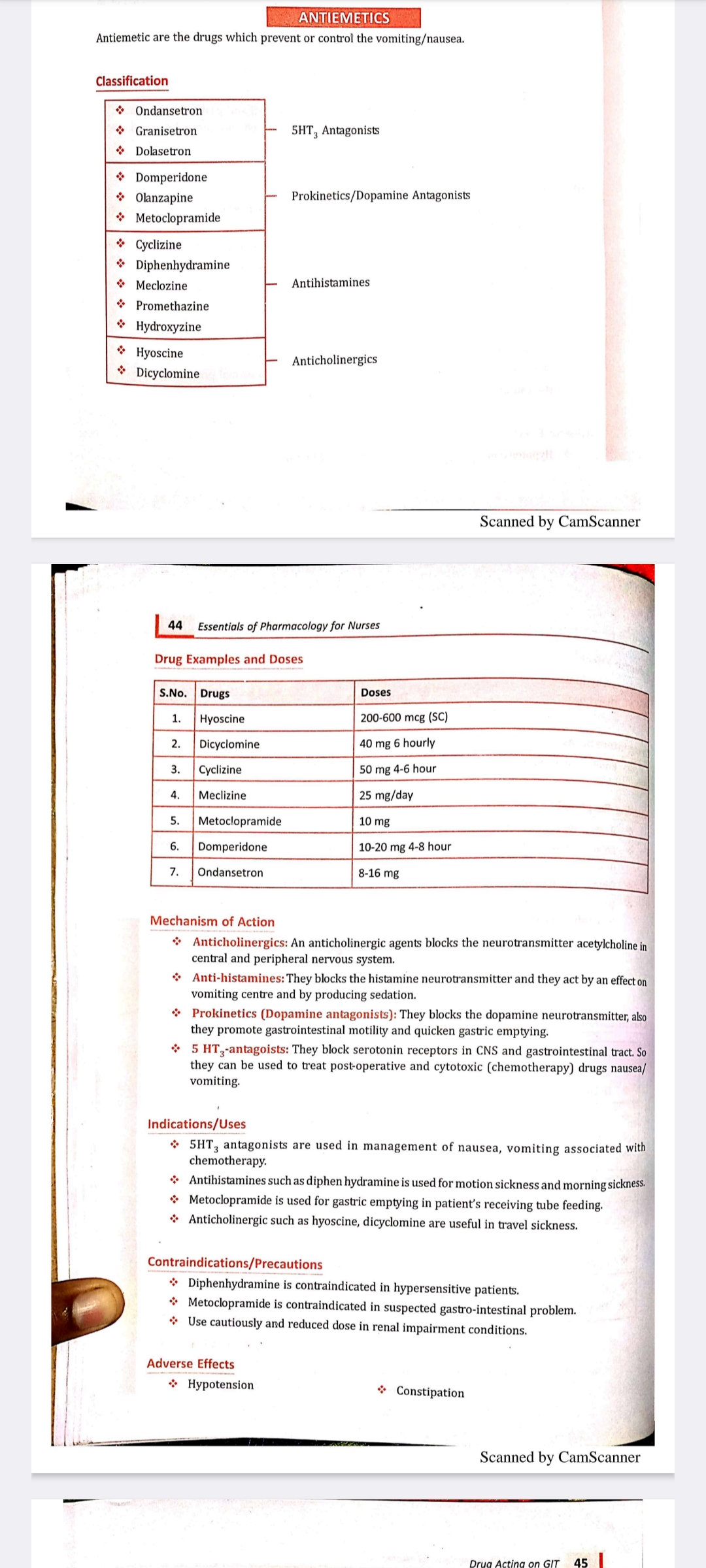
Antiemetics are drugs used to prevent or control vomiting and nausea.
Classification
| Type | Drugs |
|---|---|
| 5HT₃ Antagonists | Ondansetron, Granisetron, Dolasetron |
| Prokinetics/Dopamine Antagonists | Domperidone, Olanzapine, Metoclopramide |
| Antihistamines | Cyclizine, Diphenhydramine, Meclozine, Promethazine, Hydroxyzine |
| Anticholinergics | Hyoscine, Dicyclomine |
Insights
- 5HT₃ Antagonists: Work by blocking serotonin receptors in the central nervous system and gastrointestinal tract. Commonly used to manage nausea and vomiting related to chemotherapy.
- Prokinetics/Dopamine Antagonists: Enhance gastrointestinal motility and help with conditions requiring gastric emptying.
- Antihistamines: Often used for motion sickness and have sedative properties.
- Anticholinergics: Block acetylcholine in the nervous system, useful in treating travel sickness.
Drug Examples and Doses
| S.No. | Drugs | Doses |
|---|---|---|
| 1. | Hyoscine | 200-600 mcg (SC) |
| 2. | Dicyclomine | 40 mg 6 hourly |
| 3. | Cyclizine | 50 mg 4-6 hours |
| 4. | Meclizine | 25 mg/day |
| 5. | Metoclopramide | 10 mg |
| 6. | Domperidone | 10-20 mg 4-8 hours |
| 7. | Ondansetron | 8-16 mg |
Additional Information
- Dosage: It's essential to follow prescribed dosages to avoid adverse effects or reduced effectiveness.
Mechanism of Action
- Anticholinergics: Block neurotransmitter acetylcholine, affecting the central and peripheral nervous system.
- Antihistamines: Block histamine neurotransmitter; act on the vomiting center and produce sedation.
- Prokinetics (Dopamine Antagonists) : Block dopamine neurotransmitter, easing gastrointestinal motility and gastric emptying.
- 5HT₃ Antagonists: Block serotonin receptors; useful for post-operative and chemotherapy-induced nausea.
Indications/Uses
- 5HT₃ Antagonists: Used in chemotherapy-induced nausea and vomiting.
- Antihistamines: Effective for motion sickness and morning sickness.
- Metoclopramide: Aids gastric emptying in patients receiving tube feeding.
- Anticholinergics: Beneficial in travel sickness scenarios.
Insights
- Different classes of antiemetics target various receptors/pathways and are chosen based on specific indications.
Contraindications/Precautions
- Diphenhydramine: Avoid in patients with hypersensitivity.
- Metoclopramide: Contraindicated in suspected gastrointestinal problems.
- Renal Impairment: Caution and dose adjustment may be necessary.
Adverse Effects
- Hypotension
- Constipation
Additional Notes
- Monitoring for adverse effects is crucial to ensure patient safety during antiemetic therapy. Adjustments in therapy may be necessary based on patient responses and side effects.
Extended readings:
Essentials of Pharmacology for Nurses
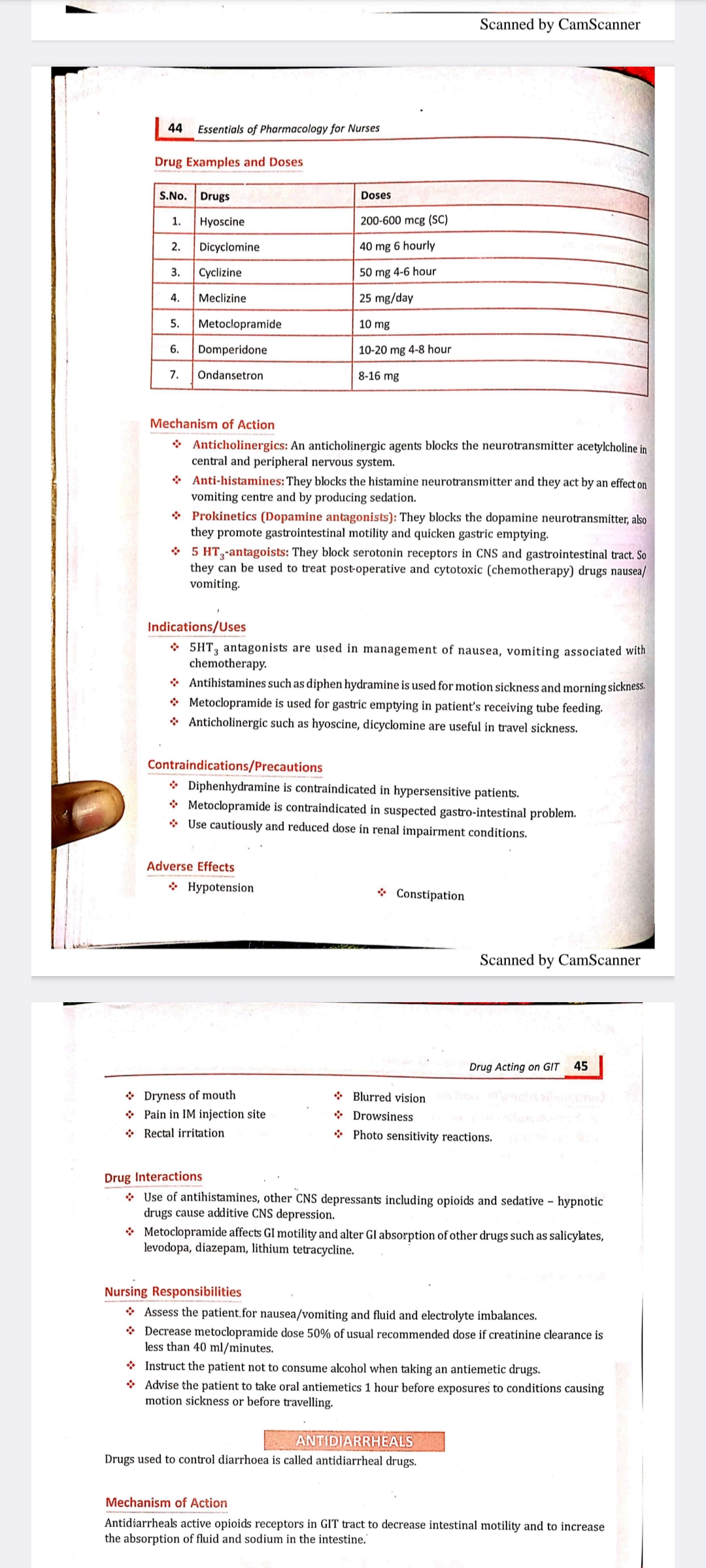
Drug Examples and Doses
| S.No. | Drugs | Doses |
|---|---|---|
| 1 | Hyoscine | 200-600 mcg (SC) |
| 2 | Dicyclomine | 40 mg every 6 hours |
| 3 | Cyclizine | 50 mg every 4-6 hours |
| 4 | Meclizine | 25 mg/day |
| 5 | Metoclopramide | 10 mg |
| 6 | Domperidone | 10-20 mg every 4-8 hours |
| 7 | Ondansetron | 8-16 mg |
Insights:
- This table lists commonly used antiemetic drugs.
- Dosing schedules are crucial in achieving therapeutic benefits while minimizing side effects.
- SC stands for subcutaneous, indicating a specific route of administration.
Mechanism of Action
-
Anticholinergics: Block the neurotransmitter acetylcholine, affecting the central and peripheral nervous systems.
Insight: Useful in conditions involving motion sickness. -
Anti-histamines: Block histamine neurotransmitters to produce sedation and affect the vomiting center.
Insight: Often used for allergy symptoms as well as nausea. -
Prokinetics (Dopamine Antagonists) : Block dopamine neurotransmitters to enhance gastric motility.
Insight: Useful in gastric emptying disorders. -
5-HT3 Antagonists: Block serotonin receptors in the CNS and gastrointestinal tract, effective against post-operative and chemotherapy-induced nausea/vomiting.
Insight: Commonly used in oncology settings to manage side effects of chemotherapy.
Indications/Uses
- 5HT3 Antagonists: Manage nausea and vomiting related to chemotherapy.
- Antihistamines (e.g., Diphenhydramine) : Used for motion and morning sickness.
- Metoclopramide: Used for gastric emptying in patients receiving tube feeding.
- Anticholinergics (e.g., Hyoscine, Dicyclomine) : Useful in travel sickness.
Contraindications/Precautions
- Diphenhydramine: Avoid in hypersensitive patients.
- Metoclopramide: Avoid in suspected gastrointestinal problems.
- Use cautiously and adjust doses in renal impairment.
Adverse Effects
- Common Adverse Effects:
- Hypotension
- Constipation
- Dryness of mouth
- Blurred vision
- Drowsiness
- Photo sensitivity reactions
Drug Interactions
- Antihistamines: Combined with other CNS depressants like opioids, cause additive CNS depression.
- Metoclopramide: Affects GI motility and alters absorption of drugs like salicylates and diazepam.
Nursing Responsibilities
- Assessment: Monitor patients for nausea/vomiting, and fluid/electrolyte imbalances.
- Dosage Adjustments: Reduce metoclopramide dose if creatinine clearance is below 40 ml/min.
- Patient Instructions: Advise against alcohol with antiemetics. Recommend taking oral antiemetics 1 hour prior to travel or motion exposure.
Antidiarrheals
- Mechanism: Act on opioid receptors to decrease intestinal motility and increase water/sodium absorption in the intestine.
Insight: Vital in managing conditions with excessive bowel movements.
Extended readings: